Wednesday 12th October at Royal Medical Society 13.00-16.30pm GMT
This event organised by the Patient Engagement Interest Group and hosted by the PM Society aimed to strike an open dialogue on pertinent issues in patient engagement among pharma, charities and agencies. It was a great success, with a strong engagement from all 64 attendees with polling responses and questions being asked throughout the afternoon.
Each of the invited guest speakers shared important perspectives and ideas on how to advance patient engagement metrics, bringing concepts to life with value-add case studies.
Important soundbites from the day included:
- Access to patients is essential when it comes to measuring patients’ experiences. As an industry, we need to consider how we can better partner with the NHS and patient advocacy groups (PAGs) as well as leverage digital.
- Participation and engagement with patients early in the process is key to the success of any patient engagement initiative, and crucial for defining what success could and should look like.
- Patient engagement has both an internal and external stakeholder measurement requirement. Think about how you’re benchmarking team effectiveness as well as programme/project effectiveness.
- There are lots of measurement tools out there from which to learn both the ‘what’ and the ‘how to’ measure. For example, R&D feels more established at this than other areas in pharma and the NHS are measuring a plethora of patient experience metrics as standard.
- Managing patients’ data securely and appropriately, being transparent about how data will be used and ensuring informed consent is all vital.
- Measurement takes time in patient engagement, especially when considering a behaviour change, make sure you are prepared for that.
- Only measure what matters and be prepared to act on what you learn, good, bad or ugly!
- Communicating what you do as the result of patients’ data and feedback is really important. Patients want to know the impact of what they’ve shared.
KEY TAKEAWAY 1: PATIENT ENGAGEMENT IS A BUSINESS IMPERATIVE
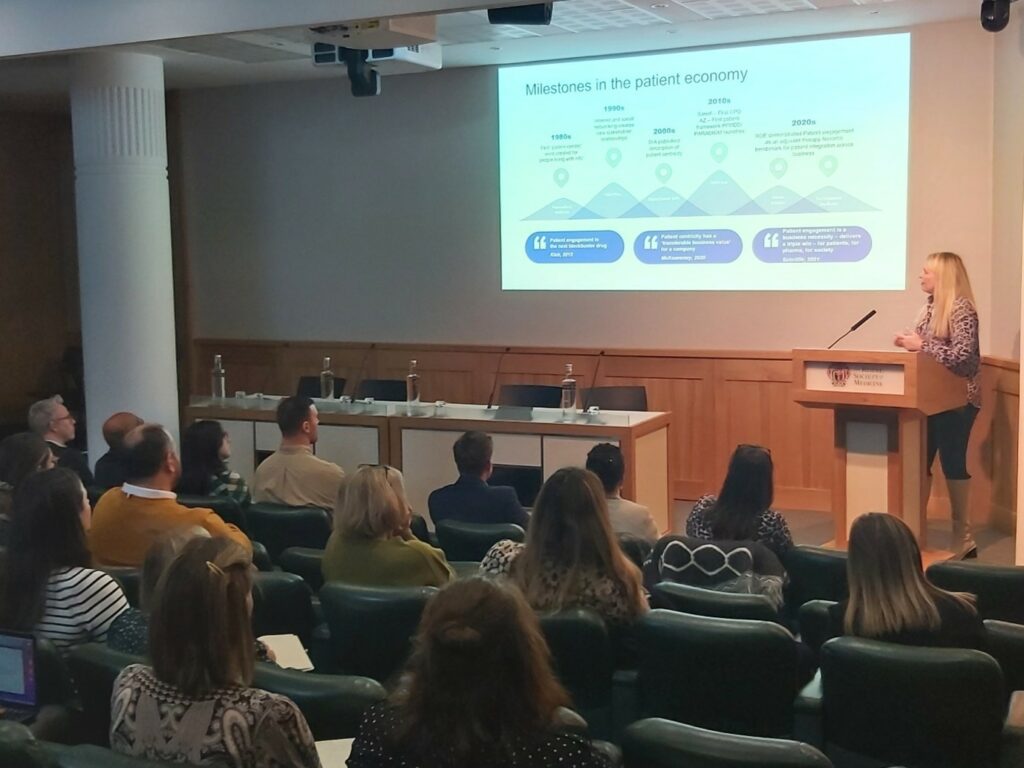
Emma Sutcliffe – Patient Engagement Consultant
Emma Sutcliffe, soon to be Global Patient Officer at Ipsen, has spent virtually her entire career working with patients and patient groups. She stated that “patient-centred healthcare does not begin when a person becomes ill” so engaging with patients early is incredibly important – in fact, we are all engaged as patients from birth, with health information and education as step one. She walked us through the evolution of patient engagement from the 1990s to now, touching on the advancements, such as the rise of the internet and digital that has allowed patients to break through to working with pharma, but also the jobs yet to be done.
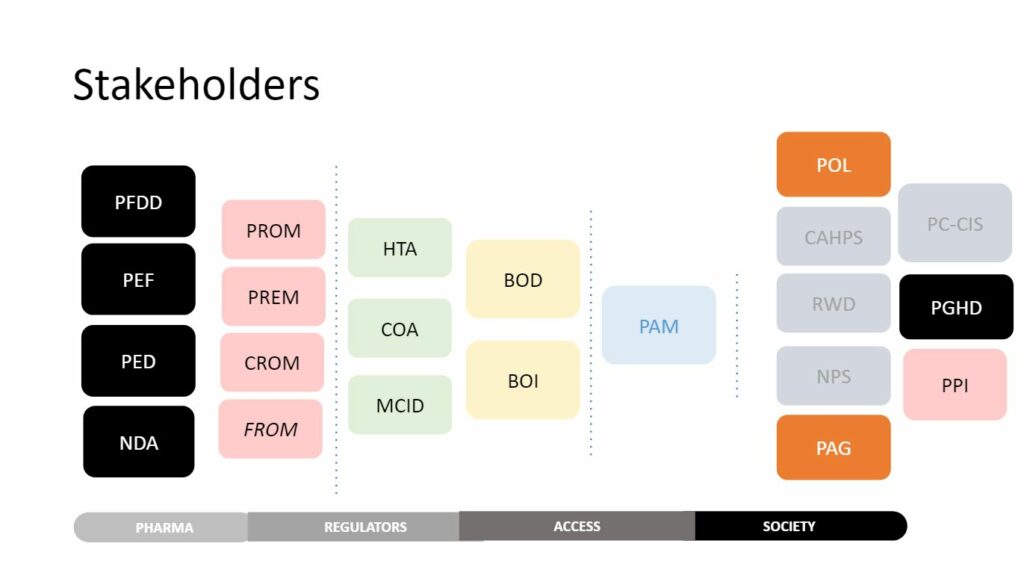
Emma is a big believer that patient engagement is not optional for pharma, stating that “patient engagement is a business necessity for pharma, delivering scientific success at lower costs with demonstrable return on investment (ROI)”, yet she spoke of the current ‘acroynm hell’ surrounding the measurement of patient engagement (summarised beautifully in the graphic below) and pharma’s focus on the patient reported outcome measure (PROM) as the key measurement to deliver evidence for regulators. However, she went on to discuss the FDA’s soon to be published paper on making the inclusion of patient experience data mandatory in all New Drug Applications, a move that shows regulators are getting serious about the importance of patient experience and putting a timeline in place for pharma to get their house in order.
So, there’s no doubt that patient engagement and its measurement are both necessary and beneficial for pharma but measuring it across the whole lifecycle isn’t easy, or yet standardised. Emma was passionate that the industry needs standardised frameworks for measurement that we can all work from, which involves co-creating robust and relevant outcomes and experience measurements that can truly capture life outcomes that are key to patients and industry. She referenced the important work by groups like the PFMD as an excellent start but urged that this must go further, stating that sometimes we must deconstruct to rebuild, referencing Dr Eric Topol’s The Creative Deconstruction of Medicine.
She rounded out her presentation, talking about patient engagement as a therapy in its own right and quoted a paper by Koch in saying, “Can you imagine if [patient engagement] reduced the need to go to hospital by this amount? It would be considered malpractice not to use it!”.
KEY TAKEAWAY 2: DESIGN THE EXPERIENCE AND MEASURE THE VALUE OF YOUR ENGAGEMENT (INCLUDING HAPPINESS!)
Jalilah Gibson – Associate Partner, PEN Partnership
Jalilah opened her presentation, rather unexpectedly, with a very cute video of a cat, and got us thinking, why do people watch cat videos? Viewing ‘cute’ things can make us happier. Research has shown that when people watch cat videos, they feel more energised and positive, while feelings of anxiety, annoyance and sadness decrease.
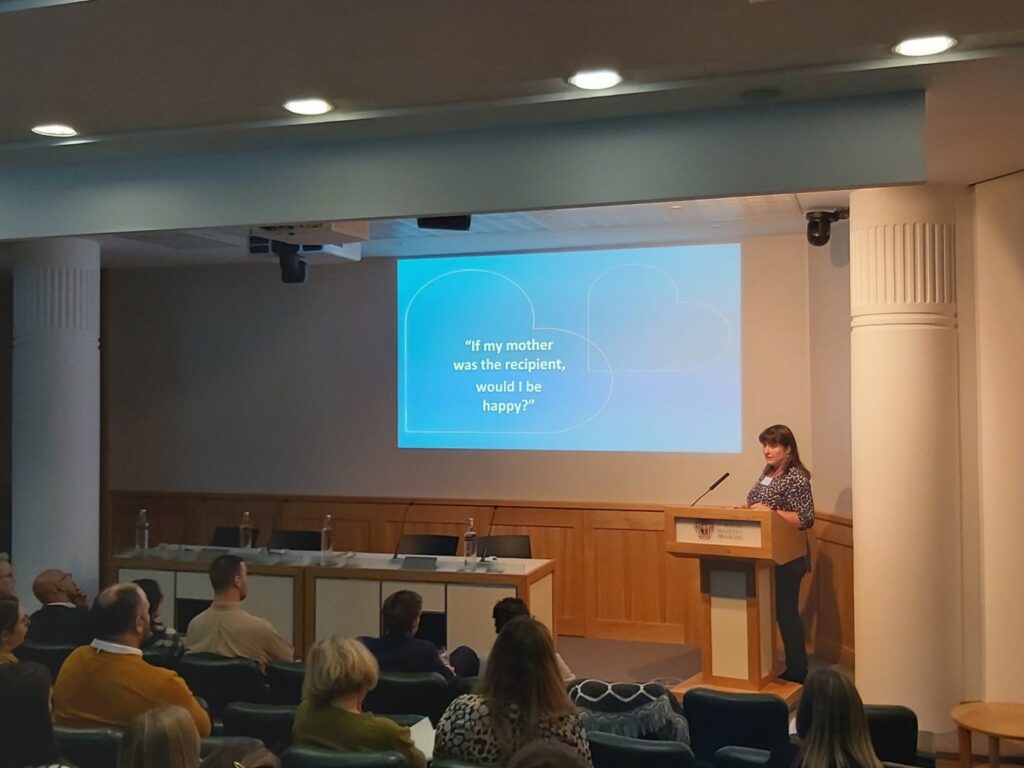
The importance of happiness also translates as a benefit to health. She referenced 3 studies where happier patients had better outcomes, such as healing faster, living longer and reducing non-adherence. Yet, despite the benefits to health, rarely do we see happiness as a KPI to measure. Jalilah talked to us about new ways to engage patients and how focusing on patient experience is a key factor to be captured for truly transforming care. When setting KPIs, she said we should be asking ourselves, “What’s the experience that you want these patients to have as a consequence of being touched by whatever you’re attempting to do?” – that’s how you set your KPIs.
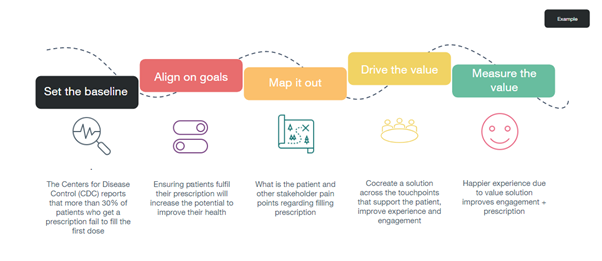
Jalilah stated that driving ‘happier’ patient experiences can deliver a return on value, explaining that it requires getting all stakeholders on board early, defining assumptions, alignment on goals, mapping the pain points, cocreating the solution and shaping new KPIs as summarised in the graphic below.
But whilst we are still battling on the best way to demonstrate ROI in pharma, digital can truly improve the patient experience through a predictive, preventative, personalised and participative approach, bringing ‘happier’ closer. Digital is key to unlocking sustainable, transformational programs and patients are ready and adopting digital solutions now. But the development of these digital initiatives requires traditionally product-centric organisations, like pharma, to adapt – creating more flexible SOPs that make the experience of engaging with pharma easier and more accessible for patients and being willing to work in a more agile way, with test & fail fast mentality.
In her closing remarks, Jalilah said, “The organisation may be willing, but they may not be ready. But the desire to change is a good place to start. Starting to design what that change looks like is absolutely the next step.”
KEY TAKEAWAY 3: INCREASE EMPATHY AND EMBED PATIENT CENTRICITY THROUGH CROSS FUNCTIONAL TRAINING
Mark Doyle – A Life in a Day; founder of The Method
Mark came to the field of patient engagement from a completely different background, following a career in acting. As the founder of The Method (derived from method acting) he has created an immersive learning experience, ‘A Life in a Day’, which is designed to get people in the pharma industry living life like a patient for a day.
The experience consists of an interactive app that sends prompts and challenges to change behaviour throughout the day, live role play with actors who take on the role of people that patients may engage with in a normal day, like a health care professional, patient support group member or even a work colleague or boss, and finally a physical kit of medical props and/or wearables to give simulations of what a patient might experience. The purpose behind the programme is to increase users’ understanding beyond the clinical impact, extending to the impacts on family, friends, work, finances, and on emotional well-being.
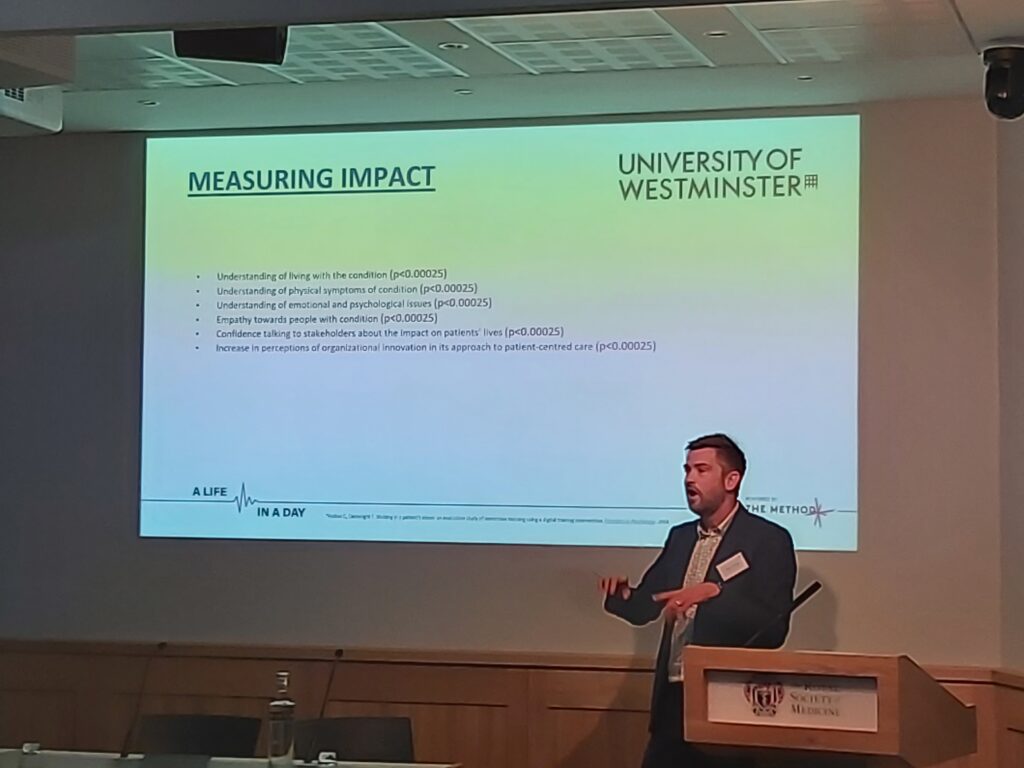
Mark touched on an important factor around measuring patient engagement, something we often think of only as an external measurement, but sometimes we also need to look at just how patient-centric we are as organisations and look to benchmark ourselves through internal measurement. By defining our baseline, we can start to understand how much work we have to do as an organisation to drive more patient centric practices across all business functions.
Feedback from participants of this experience has been extremely positive. Nevertheless, there is still a disconnect between increased empathy and actions to be taken. Mark states it is important to contextualise what driving patient centricity looks like in each business function, for example, training like this within R&D can guide patient friendly protocol design, within marketing, it can inform insights and lexicon, and for compliance it can remove barriers, increase confidence and decrease review times.
To see lasting benefits, Mark said that regular check-ins and benchmarking along the way are also important to keep us on track. We must keep reminding ourselves of the bigger picture and why we do what we do, ensuring that it isn’t lost in the day to day and we are translating patient centricity into all business functions across pharma.
KEY TAKEAWAY 4: CREATE, CAPTURE AND MEASURE PATIENT EXPERIENCE MICROMOMENTS TO UNLOCK SYSTEMS THINKING
Rachel Addy – Associate Director of Nursing, Espom and St Helier NHS Trust
The NHS has a long heritage of capturing patient experience data with several touchpoints that span from micro-moments such as beside chats to entire services dedicated to patients’ experiences, like the Patient Advice and Liaison Service (PALS). Rachel is a registered nurse and has spent 20 years at the frontline of delivering and managing patient care. She spoke on the varying methods the NHS uses to continually measure patient experiences, summarised below.
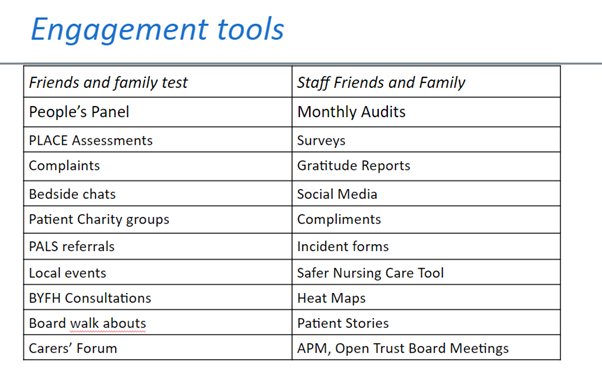
The NHS, perhaps unsurprisingly given their direct access to patients, seems far more advanced in capturing and measuring the experience of patients than in other areas of our industry and given these advancements, there is a lot to learn that we can apply to pharma. For example, Rachel spoke on the main reasons usually to blame for a poor patient experience, lack of communication in a format the patient can understand and a misalignment of expectations. This leads back to our earlier speaker’s points that, good patient engagement must begin before a patient is even ill and we must work with patients to ensure everything is delivered in a language they understand and is aligned with their expectations to meet them where they are in order to be successful.
Rachel also talked about her NHS trust’s ‘You said, we did’ campaign, where they demonstrate how they have turned patient experience data and feedback into action. This was also picked up as an important point during the panel session, that when patients choose to share their experiences with us, it is important that we communicate how that has translated into action, good or bad, this is all about building greater transparency.
Drawing upon her recent appointment to the Building Your Future Hospitals programme, focused on designing a new state of the art digitally-enabled hospital with operational excellence and a great patient experience, Rachel explained how systems thinking is crucial, as well as collaboration with all key stakeholders right from the start. She said digital will have an essential role to play and as an industry we must be prepared, not only to invest in digital patient solutions but also ensure HCPs are adequately trained to keep up with these ‘digital patients’.
Rachel’s golden rules for a robust patient engagement strategy are:
- Create a shared vision and goals
- Multi-stakeholder engagement throughout, considering equity, diversity and inclusion
- Ongoing measurement and be prepared to act on what you measure/hear
- System wide benchmarking
- Distribute reports and share learnings across the organisation
- Communicate openly to patients
KEY TAKEAWAY 5: USE MULTIPLE METHODS TO HUMANISE THE UNMET NEED AND VALIDATE BUSINESS/SOLUTION DIRECTION WITH PATIENTS
Nisa Khan – Regional Medical Affairs Manager
Jack Burton – Clinical UX Researcher, Graphite Digital
Nisa and Jack walked us through a project they collaborated on to deliver a patient reported outcome (PRO) tool to enable young people to independently monitor and capture their ongoing wellbeing and sleep patterns, to help them articulate their experiences at periodic consultations with their HCP.
Nisa firstly shared how important it is to engage and work with patients when designing and developing anything for them, as it is crucial to test assumptions and humanise the unmet need. She also stated that we need to be willing to change our plans and course correct as a result of what patients have to say, in fact, the tool they finally developed was very different to what they initially started out to do and took a little over 2 years.
Drawing on her background as a pharmacist in the NHS, Nisa noted that delivering projects routed in patient insights becomes innately more challenging from within pharma due to the lack of direct access to patients, lack of standardised processes and lack of expertise within the organisation. However, charting this project has helped create a blueprint for patient engagement within the organisation.
Throughout this project the team were able to collaborate with a patient organisation and employ multiple methods to gain data and insights, such as, surveys, focus groups, interviews, and a diary study. Nisa cautioned that while response rates can sometimes be frustratingly low, there is value in even the smallest amounts of data that you do receive. To that end, making the time and establishing the processes to collect this kind of data is business critical for overall success.
Jack added, “user research in pharma needs to be become common practice so digital offerings start creating meaningful value for patients”. There is still work to be done to educate stakeholders on the imperative need for this type of research and its indispensable value to the patient and doctor.
KEY TAKEAWAY 6: HARNESS CONSISTENT COMMUNICATION AND CONTINOUS FEEDBACK LOOPS TO TRULY DELIVER ON WHAT IS IMPORTANT TO PATIENTS

Chris Clarke, Director of Marketing and Communications, DEBRA
Chris joined us from DEBRA, a patient organisation that supports patients with Epidermolysis Bullosa (EB), an organisation that inherently has very close and direct link with patients and their families. He discussed how it was imperative that PAGs are consistently engaging with their members and sense checking at every step to ensure they are absolutely aligned with what is important to patients.
He talked on some of the methods they use to do this, for example, their governance structure requires that at least half of their board are people who’ve got EB or have a close family member with EB, they employ a formalised member engagement strategy across all functions of their organisation and also hold regular feedback forums.
He also shared his perspective on how to keep an engaged member group which included:
- Regular communications
- Understanding communication preferences to connect with members in a way that suits them
- Focusing on finding ways to reach the ‘harder to reach’ – for example, through closer collaboration with the NHS/EB centres and improving search rankings on communications
- Delivering meaningful content that is tailored to the needs of not just patients but their wider support network too, for example, family members and care givers
By looking at organisations outside of pharma, like PAGs and the NHS, who are more established at measuring patient engagement and experience data to ensure they are delivering optimal core services, there is a lot to learn. As an industry we must drive stronger long-term partnerships with PAGs and providers, establish standardised frameworks for measurement across all phases of the product lifecycle, and finally be prepared to act on feedback and data we receive.